Introduction
Physiotherapy in Winnipeg for Hand
Welcome to River East Physiotherapy's patient resource about Arthritis of the thumb injuries.
When you stop to think about how much you use your thumbs, it's easy to see why the joint where the thumb attaches to the hand can suffer from wear and tear. This joint is designed to give the thumb its rather large range of motion, but the tradeoff is that the joint suffers a lot of stress over the years. This can lead to painful osteoarthritis of this joint that may require surgical treatment as the arthritis progresses.
This guide will help you understand:
- how arthritis of the thumb develops
- how it is diagnosed
- what can be done for the condition
Anatomy
Where is the CMC joint, and what does it do?
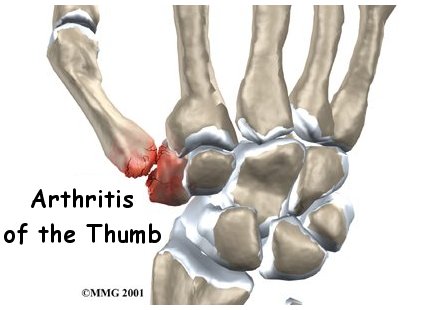
The CMC joint (an abbreviation for carpometacarpal joint) of the thumb is where the metacarpal bone of the thumb attaches to the trapezium bone of the wrist. This joint is sometimes referred to as the basal joint of the thumb. The CMC is the joint that allows you to move your thumb into your palm, a motion called opposition.
Carpometacarpal Joint

Trapezium Bone

Several ligaments hold the CMC joint together. These ligaments can be injured, such as when you sprain your thumb. The joint surfaces are covered with a material called articular cartilage. This material is the slick, spongy covering that allows one side of a joint to slide against the other joint surface easily.
Articular Cartilage

Related Document: River East Physiotherapy's Guide to Hand Anatomy
Causes
What causes arthritis of the thumb?
Arthritis is a condition in which a joint becomes inflamed (red, swollen, hot, and painful). Degenerative arthritis is a condition in which a joint deteriorates and causes pain, usually slowly over a period of many years. Doctors sometimes also describe this same condition as degenerative arthrosis. It is also called osteoarthritis.
Osteoarthritis (OA)

Injury to a joint, such as a bad sprain or fracture, can increase the risk of developing OA in the future. Such an injury could cause damage to the articular cartilage - the part of the joint that is slippery and smooth. An injury to the CMC joint of the thumb, even if it does not injure the articular cartilage directly, can alter how the joint works. After a fracture of the thumb metacarpal, the bone fragments may heal in slightly different positions. The joints may then line up differently. This is also true when the ligaments around the CMC joint are damaged by a sprain.
When an injury results in a change in the way the joint moves, the injury may increase the forces on the articular cartilage surfaces. This is similar to any mechanical device or machinery. If the mechanism is out of balance, it tends to wear out faster.

Over many years this imbalance in the joint mechanics can lead to damage on the articular surface. Articular cartilage can heal itself, but often not at the pace it needs to prevent pain. Sometimes, over time, the joint is no longer able to compensate for the increasing damage, and it begins to hurt.
It's important to remember that osteoarthritis doesn't always cause pain. If we take medical imaging (e.g. XRays) of people with pain in their hand joints and other people with zero pain, we often can see similar joint changes in both. So just because your joints are changing doesn't mean they will affect your life and your function!
Symptoms
What does arthritis of the thumb feel like?
Pain is the main problem with arthritis of any joint. This pain occurs at first only related to activity. Usually, once the activity gets underway there is not much pain, but after resting for several minutes the pain and stiffness increase. Later, when the condition worsens, pain may be present even at rest. The most noticeable problem with CMC joint arthritis is that it becomes difficult to grip anything. It causes a sharp pain at the base of the thumb in the thick part of the heel of the hand.
Base of Thumb

When the articular cartilage starts to wear off the joint surface, the joint may make a squeaking sound when moved. This sound is called crepitus. The joint often becomes stiff and doesn't move as well. Moving the thumb away from the palm may become difficult. This is referred to as a contracture.
Osteoarthritis may cause the CMC joint of the thumb to loosen and to bend back too far (hyperextension). If the middle thumb joint (MCP joint) becomes flexed and the furthest thumb joint also becomes hyperextended, the deformity is named a thumb swan neck deformity. A similar finger deformity sometimes occurs in people with finger arthritis.
Thumb Swan Neck Deformity
Related Document: River East Physiotherapy's Guide to Swan Neck Deformity of the Finger
Diagnosis
Osteoarthritis can be diagnosed by a physiotherapist - you do not need to consult your doctor first.
When you visit River East Physiotherapy, our diagnosis of CMC joint arthritis of the thumb begins with our physiotherapist taking a detailed history of the problem. Specifics about any injuries that may have occurred to the hand are important because they may suggest other reasons why the condition exists.
Following the history, our physiotherapist will examine your hand and possibly other joints in your body. We will need to see how the motion of the CMC joint and other joints have been affected.
Some patients may be referred to a doctor for further diagnosis, if your condition is complex. Once your diagnostic examination is complete, the physiotherapists at River East Physiotherapy have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
What can be done for CMC joint arthritis?
The treatment of osteoarthritis of the CMC joint of the thumb can be divided into the nonsurgical means to control the symptoms and the surgical procedures that are available to treat the condition. Surgery is usually not considered until the symptoms have become impossible to control without it.
Non-Surgical Rehabilitation
Your physiotherapist is your expert on rehabilitation, without surgery or drugs.
Treatment usually begins when the CMC joint first becomes painful. Your physiotherapist may recommend reducing the activity, or changing from occupations that require heavy repetitive gripping with the hand, may be necessary to help control the symptoms.
If your initial physiotherapy treatment plan isn't getting results, your physiotherapist may recommend you consult your doctor or pharmacist about taking mild anti-inflammatory medications, such as aspirin or ibuprofen.
Your physiotherapist at River East Physiotherapy may also work with you to obtain or create a special thumb brace or splint when needed. These devices are designed to help reduce pain, prevent deformity, or keep a thumb deformity from getting worse. A thumb stabilizer is a type of thumb splint that is often custom-made of heat-moldable plastic. It is designed to fit the forearm, wrist, and thumb. Our patients with CMC joint arthritis usually only wear the splint at night and when the joint is flared up. It should also be worn to protect the thumb during heavy or repeated hand and thumb activities.
Our primary therapeutic goal is to help you learn how to control symptoms and maximize the health of your thumb. Our physiotherapist will teach you ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs.
We will also teach you range-of-motion and stretching exercises to improve your thumb motion. Our program will likely then advance to include strength exercises for the thumb and fingers. We use dexterity and fine motor exercises to get your hand and thumb moving smoothly. Your physiotherapist will also go over tips on how you can get your day-to-day tasks done with less strain on the joint.
Although the time required for recovery varies among patients, as a guideline, you may expect to progress to a home program within four to six weeks.
Post-surgical Rehabilitation
If your initial physiotherapy treatment plan isn't getting you the results you need, your physiotherapist will refer you to your doctor. Sometimes, doctors recommend surgery.
After surgery, your hand will be bandaged with a well-padded dressing and a thumb splint for support. Your physiotherapist will design your post-operative rehabilitation program, and guide you through it.
Usually, in your post-operative physiotherapy program, the first few treatments are used to help control the pain and swelling after surgery.
Our physiotherapist will also have you begin doing exercises to help strengthen and stabilize the muscles around the thumb joint. We’ll use other exercises to improve the motor control and dexterity of your hand. Our physiotherapist will also provide tips on ways to do your activities while avoiding extra strain on the thumb joint.
When your recovery is well under way, regular visits to River East Physiotherapy will end. Although we will continue to be a resource, you will eventually be in charge of doing your exercises as part of an ongoing home program.
River East Physiotherapy provides services for physiotherapy in Winnipeg.
Physician Review
If your physiotherapist does refer you to a doctor, your doctor may take X-rays to see how much the joint is damaged.
X-Rays

This test can sometimes show how bad the degenerative arthritis has become. How much articular cartilage remains in the joint can be estimated with the X-rays.
**But remember: the amount of degeneration seen on your X-Raydoesn't correlate with the amount of pain you feel! Many people have degeneration in their joints that can be seen on an XRay, but they feel zero pain and function as well as they did 20 years earlier**

Sometimes, your doctor may recommend an injection of cortisone into the joint can give temporary relief. In Manitoba, physiotherapists do not do injections - they are done by doctors.
Cortisone is a very powerful anti-inflammatory medication. When injected into the joint itself, it can help relieve the pain. Pain relief is temporary and usually only lasts several weeks to months. There is a small risk of infection with any injection into the joint, and cortisone injections are no exception. This is one of the many reasons you should start with lower-risk treatment, such as a physiotherapy treatment program, before considering injections or surgery.
Surgery
If you and your doctor decide surgery is the right option for you, the surgical treatment for arthritis of the CMC joint includes several options. Your physiotherapist's role is to help you prepare for surgery and rehabilitation post-surgery, helping to create the conditions for the surgery to be successful. Your physiotherapist collaborates closely with your doctor and surgeon.
Here is some information about surgery.
At one time, joint replacement with an artificial joint made with silicon was very popular. Problems with silicon implants in other parts of the body have led many surgeons to return to more traditional operations such as fusion and excision arthroplasty instead. Newer artificial joints are being developed, and in the future we may see more surgeons using them.
CMC Joint Fusion
A fusion, or arthrodesis, of any joint is designed to eliminate pain by allowing the bones that make up the joint to grow together, or fuse, into one solid bone. Fusions are used in many joints and were very common before the invention of artificial joints for the replacement of arthritic joints. Even today, joint fusions are sometimes used in many different joints for treating the pain of arthritis.
A fusion of the CMC joint of the thumb is done quite often in younger people who need a strong grip or pinch more than they need the fine motion of the thumb. People who use their hands for heavy work will probably prefer a fusion over an arthroplasty (described below).
Artificial Joint Replacement (Arthroplasty)
Artificial joints are available for the CMC joint. These plastic or metal prostheses are used by some hand surgeons to replace the joint. The prosthesis acts as a spacer to fill the gap created when the arthritic surfaces of the two bones that make up the CMC joint are removed.

Excision Arthroplasty
The traditional operation for treating CMC joint arthritis is excision arthroplasty. This method has been used for many years. The purpose of excision arthroplasty is to remove the arthritic joint surfaces of the CMC joint and replace them with a cushion of material that will keep the bones separated. Most surgeons use a piece of tendon that has been rolled up and placed into the space created by removing the bone surfaces. During the healing phase after surgery, this tendon turns into tough scar tissue that forms a flexible connection between the bones, similar to a joint.

This operation is also combined with a reconstruction of the joint where tendons in the area are used to create a ligament sling between the metacarpal bone of the thumb and the carpal bone of the index finger. This helps hold the thumb in place and keeps the space between the bones from collapsing.
Portions of this document copyright MMG, LLC.